Supporting quality assurance of PLT concentrates for transfusion
Platelet concentrates are used in transfusions therapies for patients with severe thrombocytopenia. Studies have shown that the quality in terms of yield influences the platelet recovery in the recipient (1). A complete blood count using an automated hematology analyzer is widely used to ensure quality of this blood product.
Indications for PLT transfusion
Platelets are primarily involved in hemostasis, that is, the process to prevent and stop bleeding (2). They interact with each other and other cells, such as the white blood cells and vascular endothelial cells to search for sites of injury, where they become activated. Platelets also seem to be involved in the microbial host defense by detecting and regulating infections (3). When stimulated, their surface area is increased, and bioactive molecules are secreted.
The normal range for platelet count in adults is about 160–390 × 109 /L (4). Thrombocytopenia is a condition where the platelet count is below the normal range established in a population. PLT counts below 50 × 109/L can complicate surgical procedures, whereas spontaneous bleeding may occur at a PLT count below 10 × 109/L (4). In patients with low platelet counts or with platelet function defects, platelet transfusion can therefore be a lifesaving procedure (2).
Preparation of platelet concentrate
Platelet concentrates to be used in transfusion can be prepared, for example, from whole blood or by platelet apheresis. The quality of the platelet concentrate in terms of yield affects platelet recovery in the recipient (2). Extensive studies are therefore conducted to improve the yield when preparing the platelet concentrate.
Srivastava and colleagues at the Dept. of Transfusion Medicine, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India used the Medonic M-series hematology system to determine pre-donation platelet count in donors before platelets were collected by apheresis (6). Pre-donation platelet count was shown to statistically correlate with platelet yield. These findings were confirmed by Malod and coworkers at the Dept. of Transfusion Medicine, Malabar Cancer Centre, Thalassery, Kerala, India, using the Medonic M-series M32M hematology system (7).
In a study conducted to optimize the platelet concentration in platelet-rich plasma, Kirimlioglu and Yapici at the Akdeniz University, Faculty of Medicine, Department of Histology and Embryology, Antalya, Türkiye and the Çallı Meydan Medical Center, Clinic of Orthopedic Traumatology, Antalya, Türkiye, respectively, used the Medonic M-series M16M hematology system to determine platelet count in the donated venous whole blood as well as in the buffy coat after centrifugation (8). The results show that the amount of used blood volume correlates with the amount of obtained platelets in final product.
Automated hematology testing in blood bank applications
Hematology testing is commonly used in pre-donation assessment of the donor, pre-transfusion assessment of the patient, as well as in quality monitoring of the blood product.
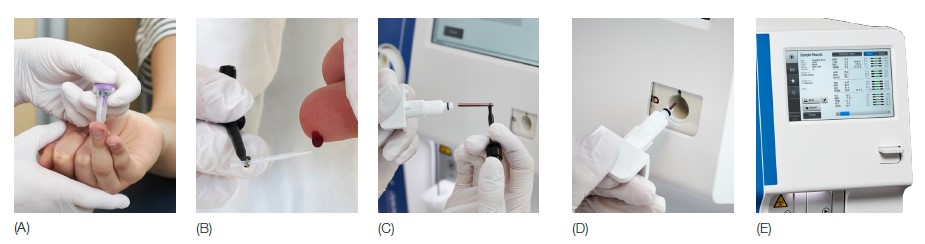
Complete blood count from one drop of blood
Medonic M32 hematology system reports a complete blood count, including a WBC differential count in about one minute. Analyzer models featuring the MPA method allows hematology testing from capillary blood collected from a fingerstick sample, saving the vein for the actual donation (Fig 1).
For accurate determination of PLT count in the critically low range, as in the case of severe thrombocytopenia, Medonic M32 features an PLT extended counting time functionality. When activated, the analyzer will count three times as many platelets to ensure a sufficiently large number to allow an accurate determination of the PLT count.
These functionalities make Medonic M32 well-suited for use in both donor and recipient assessments.
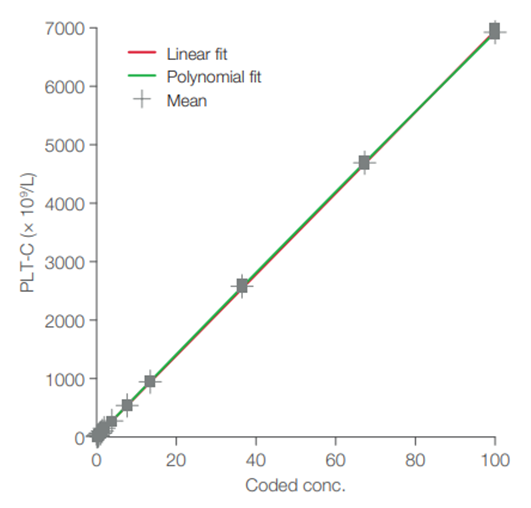
Blood bank application for PLT concentrates
The Medonic M32 blood bank application for platelet concentrates resides in the Medonic M32 analyzer as a special analysis profile. This blood bank profile is named PLT-C (i.e., platelet concentrate). The profile is pre-installed in the analyzer and can be activated by the service technician upon delivery of the instrument. Plots of recovered versus theoretical values show good conformity over the linearity range (Fig 2). The results indicate that Medonic M32 can be a useful tool for efficient control of platelet concentrates.
Learn more
Learn more about Boule blood bank applications from the white paper Hematology testing in blood banking and transfusion applications.
References
- Norol et al. Platelet Transfusion: A Dose-Response Study. Blood 92, 1448–1453 (1998).
- Khan and Anwer. Platelet Transfusion. StatPearls, StatPearls Publishing; Treasure Island (FL) (2023).
- Assinger, A. Platelets and Infection – An Emerging Role of Platelets in Viral Infection. Front Immunol 5, 649 (2014).
- Mayo Clinic Laboratories. Rochester Interpretive Handbook (2021).
- Kuter, D.J. Treatment of chemotherapy-induced thrombocytopenia in patients with non-hematologic malignancies. Haematologica 107, 1243–1263 (2022).
- Srivastava et al. Effect of donor parameters and cell separators on yield of apheresis platelet and their impact on corrected count increment in aplastic anemia patients. Asian J Transfus Sci 17, 246-250 (2023).
- Malod et al. Predicting donor-related factors for high platelet yield donations by classification and regression tree analysis. Hematol Transfus Cell Ther 45, 217−223 (2023).
- Kirimlioglu and Yapici. Determination of the optimum platelet-rich plasma method for the essential amount of platelets. Ann Med Res 30, 1037–1040 (2023).
