Ensure reliability and cost-efficiency in decentralized diagnostic testing
With today’s customer-centric approach to healthcare, decentralized testing is growing rapidly. In such clinical settings, capillary samples are typically used, yet laboratory reference values are commonly set using venous blood. This article highlights sources of discrepancies between capillary and venous blood samples, and procedures to obtain reliable results with capillary samples are proposed. Combination of equipment for cost-efficiency in diagnostic testing at the point of care is discussed.
Introduction
Traditionally, biomedical analyses are conducted at large hospital laboratories away from the patient. However, technology advancements have enabled equipment manufacturers to provide test devises for use in a decentralized clinical setting closer to the patient but that can produce the quality analysis results expected from a hospital laboratory. This evolution is propelling the market trend that indicates a move from centralized clinical diagnostic testing to testing at the point of care (1). Furthermore, decentralized diagnostic testing solutions facilitate health assessments at the doctor’s office, shortening time to diagnosis and initiation of treatment. Early diagnosis and treatment not only provide health benefits for the patient but can also offer health economic benefits to the healthcare facility. Pre-analytic risk factors such as blood coagulation can also be minimized when time between sampling and analysis is shortened.
Hematology testing at the point of care
In general screenings of patients’ health status, a complete blood count (CBC) is typically requested. Today, such an analysis is performed using an automated hematology analyzer. In addition to reporting the number of oxygen-carrying red blood cells (RBCs), platelets (PLTs) that help blood clot, and white blood cells (WBCs) of the immune system, the analyzer also measures the oxygen-containing hemoglobin (HGB) and determines a range of other parameters such as the mean RBC and PLT volumes and hematocrit (HCT), that is, the red blood cell-to-plasma ratio.
Depending on the differentiation of the WBCs, hematology analyzers are divided into 3-part systems and 5-part systems (2). In addition to a CBC, a 5-part analysis differentiates the WBCs into their five mains subgroups, neutrophils (NEU), lymphocytes (LYM), monocytes (MONO), eosinophils (EOS), and basophils (BASO), while a 3-part analyzer combines NEU (60% of WBC count), EOS (1%–4% of WBC count), and BASO 0.5%–1% of WBC count) into granulocytes (GRAN), of which NEUs constitute the largest part. For fever investigations, for example, the NEU and LYM counts will answer the question of a viral infection or a bacterial infection that can be treated with antibiotics.
In comparison to a 5-part instrument, a 3-part hematology system is typically more cost-efficient and is therefore many times used as a workhorse in general health screenings. Based on robust technologies that commonly require less maintenance than what is typical for a 5-part analyzer, a 3-part analyzer is often the instrument of choice for the physician’s office laboratory (POL). In addition to simplicity of use, a prerequisite often mentioned for use of an analyzer in such a clinical setting is the support of small sample volumes.
With the development of the very first automated European blood cell counter in 1956, Boule has a strong heritage in hematology diagnostics. The company has a long experience in designing hematology systems and Boule’s cell count processes have been tested and optimized for decades for robust and reliable analysis results. Equipped with the micro-pipette adapter (MPA) inlet, the Swelab Alfa Plus hematology analyzer reports a complete blood count (CBC), including a 3-part WBC differential, from just one drop of blood in about one minute (Fig 1).

Fig 1. Swelab™ Alfa Plus hematology analyzer provides a complete blood count from a simple finger-stick capillary sample in just one minute.
Types of blood and their use
To become oxygenated, blood is pumped from the right side of the heart to the lungs where it leaves carbon dioxide and takes up oxygen. The now oxygenated blood is pumped from the left side of the heart out in the body through the arteries, while the deoxygenated blood is pumped back to the right side of the heart through the veins (Fig 2). Nutrients are picked up when the blood flows though the intestines and waste is filtered out from the blood when flowing through the kidneys. The smallest arteries and veins are joined in capillary beds, where the exchange of blood contents is taking place. In the capillary beds, oxygen and nutrients are distributed out to the body’s tissues and organs and carbon dioxide and other waste products from the cells are picked up for disposal. Capillary blood is therefore a combination of arterial and venous blood.
Typically, arterial blood is used for determination of arterial blood gases, while venous blood is recommended for laboratory testing. Accordingly, laboratory reference values are commonly set using venous blood samples. However, there are circumstances where capillary blood can be preferred. For example, capillary blood sampling can be an option for patients that are hard to puncture such as elderly. As a fingerstick often is easier on the patient, capillary sampling is typically also used in pediatrics. Under certain conditions, for example, in cases of leukemia or infectious diseases that affect the blood cells (e.g., dengue fever or malaria infection), close monitoring of the patient’s blood status might be required. For cases that require frequent blood testing, capillary blood sampling can be preferred over venous blood withdrawal.
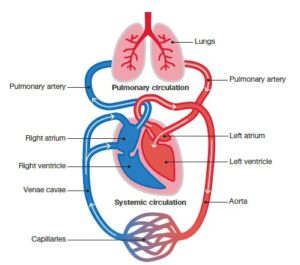
Fig 2. Overview of the vascular system.
Performing a fingerstick: what can affect the results The relevance of using capillary blood in diagnostic testing is sometimes debated. In addition to differences in content between capillary blood and venous blood, improper preparation and blood collection procedures can also cause discrepancies between capillary and venous blood values.
In hematology, for example, the tendency of the PLTs to clump or adhere to tissue and to the walls of the capillary sampling tube can affect the test results. Consequently, the PLT count can be 5% to 10% lower in capillary blood, and if PLT clumping occurs, the lymphocyte count can be falsely elevated. It is therefore important to follow general guidelines for capillary blood sample collection to obtain reliable results (3).
The sampling procedure should ensure a good blood flow. A deep and firm puncture allows for free-flowing drops of blood. To increase the blood flow, the site for puncture can be warmed for 3 to 5 min before disinfection and puncture of the skin. To minimize interstitial and intracellular fluids in the sample, the first drop of blood should be wiped off with a clean tissue. The sample should be analyzed directly after collection, and for optimal results, no longer than 10 min from collection.
Complete blood count from one drop of blood
Swelab Alfa Plus automated hematology system is trusted for its high reliability and ease-of-use. From the small doctor’s office laboratory to the medium-sized clinical laboratory, the system delivers a complete blood count (CBC), including a 3-part WBC differential, with outstanding speed and precision.

Fig 3. Swelab Alfa Plus automated hematology system equipped with the micro-pipette-adapter (MPA) inlet for capillary samples is designed for
blood testing in a decentralized clinical setting. (A) Make a deep and firm skin puncture. (B) Collect 20 μL blood into the K2EDTA-coated micropipettes.
(C) Slide the tube into the adapter. (D) Insert the adapter into the analyzer. (E) CBC results are viewable on the display in about one
minute.
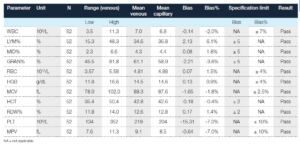
Table 1. Comparison of capillary blood collected in micro-pipettes and analyzed in MPA mode versus venous blood collected in bullet tube
and analyzed in OT mode (4)
Dr. Irlanda Mohammad Idzham about the MPA functionality
” The small volume of capillary sample is important when handling infectious diseases.
Capillary sampling is also less fearful for children, feeling more comfortable when holding
them by the finger rather than grabbing their arm. Therefore, the MPA functionality is the
most important feature of Swelab Alfa Plus. This instrument is also the smallest on the
market, and easy to use. The results are accurate and consistent, which gives confident
to the clinician. The capillary hook holder facilitates sample handling.”
Dr. Irlanda Mohd Idzham, Klinik Idzham Sdn Bhd, Kuala Lumpur, Malaysia

Dr. Irlanda Mohd Idzham, Klinik Idzham Sdn Bhd, Kuala Lumpur, Malaysia
Hematology analyzers: 3-part or 5-part, that is the question
Although each WBC sub-type provides information that helps diagnose blood-related conditions, a 3-part instrument will provide sufficient information for general screenings in a typical POL setting. For specialty laboratories, however, a 5-part instrument can provide a more detailed and targeted assessment of the blood status. To distinguish EOS and BASO from NEU, for example, a 5-part differentiation is mandatory.
However, the cost for a typical 5-part instrument can be two to three times higher (20,000 to 50,000 USD) than for a 3-part instrument (less than 10,000 USD). In addition, a 5-part WBC differential often requires more reagents than a 3-part WBC differential, also increasing the cost per test from below 1 USD/test for a 3-part system to 1.5 to 3 USD/test for a 5-part system. Yet, government reimbursements commonly do not consider whether WBCs are differentiated into 3 or 5 parts. Hence, 5-part instruments are typically used by oncology or allergy clinics that can justify the higher cost associated with obtaining absolute EOS and BASO counts.
Gain cost-efficiency in hematology testing
Many clinical laboratories are challenged with high testing cost that reduce their margins. At the same time, an extensive list of reported parameters might be required for the specific clinical setting and an attractive test offering can be a prerequisite to stay competitive on the diagnostic testing market. Such laboratories might be referred to the use of a more expensive 5-part hematology system, although the larger part of incoming sample requests might be for CBC results only. For such scenarios, the combination of the less expensive 3-part instruments with a small point-of-care (POC) device, such as the spinit® system, can be the solution. In addition to test discs for rapid and quantitative
measurement of C-reactive protein (CRP) and glycated hemoglobin A1c (HbA1c), the spinit product portfolio includes a test disc for total and 5-part differential counts of the WBCs. That means, the same instrument allows performing both hematology and clinical chemistry analyses in short process time. No calibration and little or no maintenance requirements contribute to an easy and efficient instrument use. Instrument operation is straightforward, just insert a disc and follow the on-screen instructions to perform a test (Fig 4). While the 3-part hematology analyzer can be used for the larger part of all samples, requiring a simple CBC only, the spinit BC test can be used with samples for which a 5-part WBC differential is requested. The spinit BC test report comprises total WBC count as well as percentage and absolute NEU, LYM, MONO, EOS, and BASO counts. Furthermore, spinit CRP can be used to confirm samples indicated as infectious in the 3-part WBC differential. As HbA1c values can be affected by HGB levels, the
spinit HbA1c disc, reporting also plasma glucose, can be used together with HGB results from the hematology analyzer for assessment of glycemic control in diabetic patients (5). Results are displayed for on-screen view or they can be exported for print or for transfer to a laboratory information system (LIS).

Fig 4. The spinit test discs integrate everything required for sample
analysis, just collect blood, apply to disc, and insert in instrument. Results
will be displayed in a few minutes.
Conclusion
Market trends indicate an increase in near-patient diagnostic testing. However, testing in a typical physician’s office laboratory pose challenges related to instrument size, supported sample types, and complexity of the included technology. With its compact design, Boule’s automated Swelab Alfa Plus hematology system is well suited for the smaller laboratory. Equipped with the MPA inlet for capillary samples, the analyzer reports a complete blood count including a 3-part WBC differential from one drop of blood in about one minute. A robust system design keeps maintenance needs to a minimum. Well-proven cell count processes ensure accurate and reliable analysis results. Combined, Boule 3-part hematology and spinit POC systems can provide a costefficient solution for near-patient diagnostic testing.
References
1. Report: The Worldwide Market for Point-of-Care. Kalorama. Feb 2018.
2. Whitepaper: Hematology analyzers – 3-part or 5-part, that is the question. Boule Diagnostics, 31183, Edition 2 (2019).
3. Instruction: Capillary blood sample collection. Boule Diagnostics, 33353, Edition 1 (2019).
4. Application note: Comparison of capillary and venous blood samples on Swelab Alfa Plus hematology analyzer. Boule Diagnostics, 31783, Edition 1 (2019).
5. Bae et al. Hemoglobin A1c values are affected by hemoglobin level and gender in non-anemic Koreans. J Diabetes Investig 5, 60–65 (2014).
Boule 3-part hematology testing in combination with spinit BC 5-part analysis can provide cost-benefits compared with hematology testing on a 5-part analyzer
Less upfront payment
The investment cost of a combination of the 3-part hematology analyzer and the spinit analyzer can be about half the cost of a 5-part analyzer.
Lower testing cost
Testing cost for hematology analysis using a 3-part analyzer with spinit BC analysis included for 5% of all samples can be about half the testing cost compared with all samples tested using a 5-part analyzer.
